 Scleroderma, a complex autoimmune disorder, is characterized by the abnormal growth of collagen, leading to the hardening and tightening of the skin and connective tissues. This condition can significantly impact various bodily systems, including the skin, blood vessels, and internal organs. Understanding scleroderma is crucial for early diagnosis and effective management, as it can lead to serious complications if left untreated. This article delves into the various aspects of scleroderma, including its types, symptoms, causes, diagnosis, treatment options, and living with the condition.
Scleroderma, a complex autoimmune disorder, is characterized by the abnormal growth of collagen, leading to the hardening and tightening of the skin and connective tissues. This condition can significantly impact various bodily systems, including the skin, blood vessels, and internal organs. Understanding scleroderma is crucial for early diagnosis and effective management, as it can lead to serious complications if left untreated. This article delves into the various aspects of scleroderma, including its types, symptoms, causes, diagnosis, treatment options, and living with the condition.
Understanding Scleroderma
Scleroderma, derived from the Greek words “sclero” meaning hard and “derma” meaning skin, is a rare rheumatic disease that primarily affects the connective tissues. It manifests through excessive collagen production, resulting in fibrosis, which can either be localized to the skin or systemic, affecting multiple organs. The disease is not contagious and primarily affects women, particularly those aged between 30 and 50.
Types of Scleroderma
Scleroderma is broadly categorized into two main types: localized and systemic. Each type has its own subcategories, which are essential for understanding the specific manifestations and potential complications.
-
- Localized Scleroderma: This form primarily affects the skin and underlying tissues without involving major organs. It is often characterized by patches of thickened skin and can improve over time.
- Morphea: Presents as oval-shaped patches of thickened skin, often with a red border.
- Linear Scleroderma: Appears as bands of thickened skin, typically affecting children and can lead to limb underdevelopment.
- Systemic Scleroderma: This more severe form can affect the skin as well as internal organs, including the heart, lungs, kidneys, and gastrointestinal tract. It is further divided into:
- Limited Scleroderma (CREST Syndrome): Characterized by skin thickening primarily in the fingers and face, with less severe internal organ involvement.
- Diffuse Scleroderma: Involves rapid skin thickening and significant internal organ damage, often leading to serious complications.
- Localized Scleroderma: This form primarily affects the skin and underlying tissues without involving major organs. It is often characterized by patches of thickened skin and can improve over time.
Symptoms of Scleroderma
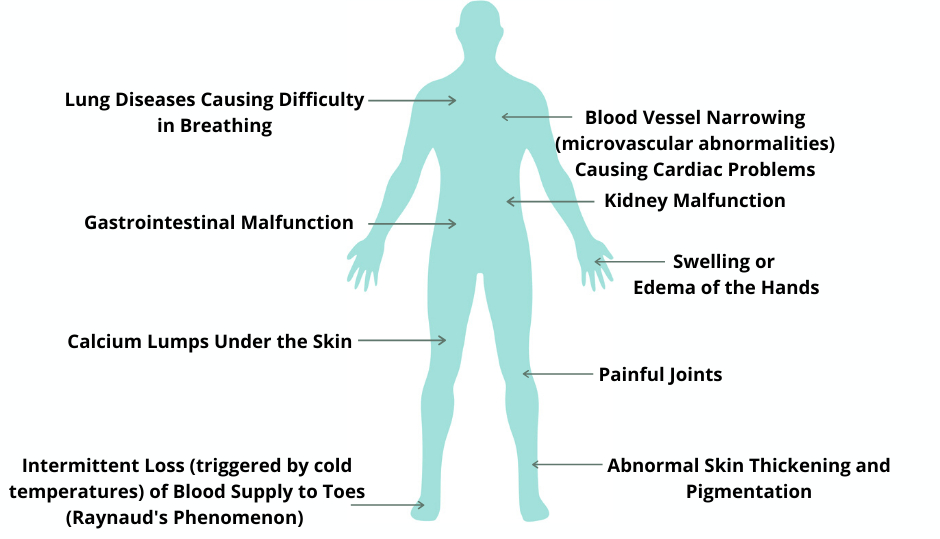
The symptoms of scleroderma can vary widely depending on the type and severity of the disease. While some individuals may experience mild symptoms, others may face life-threatening complications.
Skin-Related Symptoms
One of the hallmark signs of scleroderma is the hardening and tightening of the skin. Common skin-related symptoms include:
-
- Thickened Skin: Often first noticed on the fingers, hands, and face, the skin may appear shiny and tight.
- Raynaud’s Phenomenon: A condition where blood vessels in the fingers and toes constrict excessively in response to cold or stress, leading to color changes and numbness.
- Telangiectasia: Small red spots caused by dilated blood vessels, commonly seen on the face and hands.
Internal Organ Symptoms
When scleroderma affects internal organs, it can lead to a range of symptoms, including:
-
- Digestive Issues: Difficulty swallowing, heartburn, bloating, and changes in bowel habits.
- Respiratory Problems: Shortness of breath and persistent cough due to lung involvement.
- Cardiovascular Symptoms: Irregular heartbeats and increased blood pressure in the lungs, known as pulmonary hypertension.
Causes of Scleroderma
The exact cause of scleroderma remains unknown, but several factors are believed to contribute to its development:
- Genetic Factors: Certain genetic predispositions may increase the likelihood of developing scleroderma, although it is not directly inherited.
- Environmental Triggers: Exposure to certain chemicals, such as silica dust or polyvinyl chloride, may trigger the onset of the disease.
- Immune System Dysfunction: An abnormal immune response may lead to excessive collagen production and subsequent tissue damage.
Risk Factors
While anyone can develop scleroderma, certain groups are at a higher risk:
- Gender: Women are significantly more likely to be diagnosed with scleroderma than men.
- Age: The disease typically manifests between the ages of 30 and 50.
- Ethnicity: African Americans may experience more severe symptoms and earlier onset compared to other racial groups.
Diagnosis of Scleroderma
Diagnosing scleroderma can be challenging due to the variability of symptoms and their overlap with other conditions. A comprehensive approach is essential for accurate diagnosis.
Clinical Evaluation
A healthcare provider will conduct a thorough physical examination and review the patient’s medical history. Key aspects of the evaluation include:
-
- Skin Examination: Assessing for thickened skin, color changes, and other characteristic signs.
- Blood Tests: Tests such as the antinuclear antibody (ANA) panel can help identify autoimmune activity.
- Imaging Studies: X-rays, CT scans, and echocardiograms may be used to evaluate organ involvement.
Referral to Specialists
In many cases, patients may be referred to a rheumatologist, a specialist in autoimmune diseases, for further evaluation and management.
Treatment Options for Scleroderma
While there is currently no cure for scleroderma, various treatment options can help manage symptoms and improve quality of life.
Medications
-
- Immunosuppressants: These drugs help reduce the immune system’s activity, thereby decreasing inflammation and collagen production.
- Corticosteroids: Used to manage inflammation and control symptoms, particularly in acute phases of the disease.
- Symptomatic Treatments: Medications to address specific symptoms, such as heartburn or high blood pressure, are often prescribed.
Physical and Occupational Therapy
Therapies aimed at improving mobility and function can be beneficial for individuals with scleroderma. Physical therapy can help maintain joint flexibility, while occupational therapy can assist with daily living activities.
Lifestyle Modifications
Adopting certain lifestyle changes can also aid in managing scleroderma:
-
- Skin Care: Regular use of moisturizers can help alleviate dryness and stiffness.
- Dietary Adjustments: A balanced diet rich in nutrients can support overall health and well-being.
- Stress Management: Techniques such as yoga, meditation, and deep breathing can help reduce stress, which may exacerbate symptoms.
Living with Scleroderma
Coping with scleroderma can be challenging, but with the right support and resources, individuals can lead fulfilling lives.
Support Networks
Connecting with support groups and organizations dedicated to scleroderma can provide valuable resources and emotional support. Sharing experiences with others facing similar challenges can foster a sense of community and understanding.
Regular Monitoring
Ongoing medical care is crucial for managing scleroderma effectively. Regular check-ups with healthcare providers can help monitor disease progression and adjust treatment plans as needed.
Mental Health Considerations
Living with a chronic condition can take a toll on mental health. Seeking counseling or therapy can be beneficial for managing anxiety, depression, or feelings of isolation.
Scleroderma is a complex autoimmune disorder that requires a comprehensive understanding for effective management. By recognizing the symptoms, understanding the types, and seeking timely medical intervention, individuals can navigate the challenges posed by this condition. While there is no cure, advancements in treatment options and supportive care can significantly enhance the quality of life for those affected by scleroderma. With continued research and awareness, there is hope for improved outcomes and a better understanding of this multifaceted disease.
We help Patients with All Sorts of Skin, Hair, and Nail Challenges
General Dermatology encompasses the complete range of disease and conditions of skin, hair and nails.Our goal is to help each of our patients achieve healthy, beautiful skin through proper skin care, skin surveillance, and accurate diagnosis and treatment of skin disease.
> Learn More
Contact Us (859) 283-1033 for a Consultation
—
 About Dermatology Associates of Northern Kentucky
About Dermatology Associates of Northern Kentucky
Dermatology Associates of Northern Kentucky offers a range of services for all age groups, including general and pediatric dermatology, dermatologic surgery, Mohs Micrographic surgery, laser and cosmetic procedures, and Dermatopathology.
> Learn More

 About Dermatology Associates of Northern Kentucky
About Dermatology Associates of Northern Kentucky